Updated: January 6, 2025
Published: April 14, 2020
eHealth has the great potential to deal with some burning issues faced by today’s society. As never before, we are in need of accessible, efficient, and affordable healthcare services. Innovative telehealth software development upholds lasting value for both medical personnel and patients. Remote care, doctor’s availability and convenience are only a few of numerous advantages to see. In this article, we’ll discuss what challenges can be solved, common features and required compliance regulations for telehealth software development.
List of the Content
- Challenges that telehealth software development should solve
- Features to implement while building a telehealth app
- HIPAA compliance for telehealth software development
- Telehealth software development trends
- Conclusion
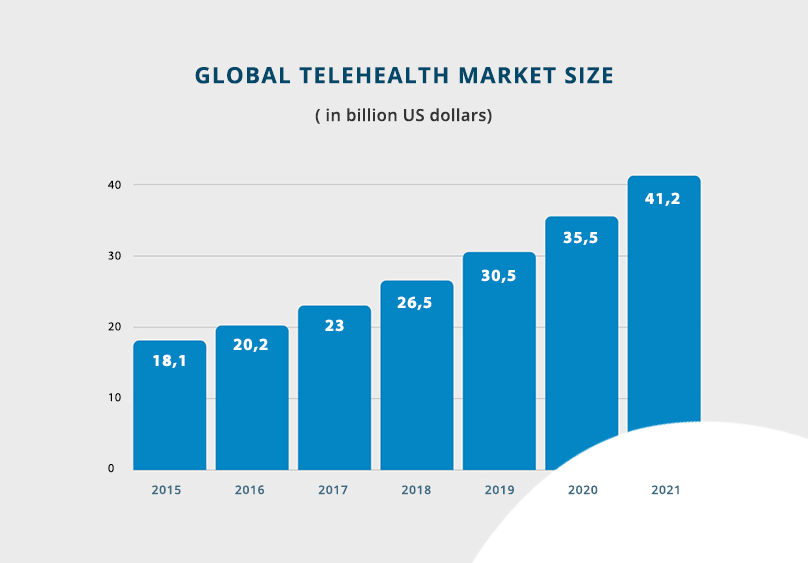
According to the statistics, the global telehealth market is expected to grow to $41.2 billion in 2021 in comparison with $18.1 billion in 2015. It is obvious that growth is driven by fast-developing technology innovations. Furthermore, such aspects as the shortage of healthcare professionals, the aging of the population, the increase in chronic diseases, growing need for outpatient and preventative care make governments and healthcare providers adopt new approaches. They explore all the possibilities for enhancing the personnel’s productivity and overall care efficiency. For example, 65% of US physicians that practice outpatient care and 40% of medical specialists in inpatient care services have already supported eHealth applications and use it on a regular basis. The others state that 90% of eHealth investments are planned to happen within the next 12 to 18 months.
Telehealth software systems can cover three major types of services:
Store-and-forward – the approach supports the data exchange between medical staff, patients, laboratory professionals, pharmacies, etc. The functional and secure software allows them to share such sensitive data as patients’ medical records, lab tests, images and videos, and prescriptions.
Remote monitoring – the valuable method to assure frequent monitoring, efficient treatment, reduce costs and increase patient satisfaction. Such service is suitable for patients with high risks, chronic conditions, recently released from hospitals, etc. A variety of technological devices help to monitor clinical signs and patients’ health conditions at the distance and keep in touch 24/7.
Real-time interaction – we can’t underestimate the benefits of communication via chat or real-time video remote visits by doctors. It is mainly used for primary and preventative care, consultations, follow-up visits, psychological support, etc. The point is that Skype or FaceTime won’t be appropriate since it has to be conducted over the HIPAA-compliant telehealth software platform.
As a result, telehealth software development isn’t just growing in popularity but has become the absolute necessity of today’s healthcare. It gives access to efficient and affordable care services. About 74% of US citizens are interested in receiving healthcare via software systems. Those who have already used it acknowledge good quality or even better than in-person visits, whereas the cost remains lower.
In their turn, healthcare providers invest in telehealth software development that can meet specific user needs and compliance regulations, including security. Taking the example of the Doctor On Demand app, we’ll discuss what challenges can be solved, common features for these software platforms, and compliance regulations.
WHAT ARE CHALLENGES THAT THE TELEHEALTH SOFTWARE DEVELOPMENT SHOULD SOLVE
“…the highest attainable standard of health as a fundamental right of every human being.” the WHO Constitution (1946)
At present, governments have to focus on making it a priority to incorporate telehealth into the existing healthcare systems. Many countries work on adopting telehealth software development to provide better care and support medical practices. It isn’t hard to prove the point that eHealth is vital for today’s society enclosing the same four fundamentals of the right to health:
Increasing accessibility
Patients have the right to access healthcare services where and when they need them. The eHealth software is the additional ability to ensure those rights. If we consider the rural communities, there is an apparent lack of specialists, including primary care physicians. Americans living in rural areas are seven times more likely to report that they were not able to get care when needed in comparison to urban areas at three times. Using the Doctor On Demand app, they are able to have an appointment with their physician just in a few minutes.
Making healthcare more affordable
Healthcare must be both physically and economically accessible. Due to the rising costs of services, telehealth software development is given high priority by governments of different countries. They found eHealth as a practical and cheaper alternative to monitor patients with chronic diseases, provide consultations, make prescriptions, share lab tests, etc. In fact, each prevented emergency case with eHealth can make savings from $309 to more than $1500 per visit.
Enabling the more patient-centric approach
This challenge is related to medical ethics and requires a people-centered approach. Putting the needs of people at the center of medical systems helps to advance care quality. With the help of telehealth software systems, patients are empowered to take more active and responsible roles in their health. For instance, patients feel more comfortable dealing with anxiety or depression via eHealth applications. Licensed psychologists have the ability to provide behavioral and/or mental health care according to international compliance standards and guarantee confidentiality to their patients.
Quality
Maintaining a good quality of healthcare is a real challenge for every generation. The integration of technology in medicine has opened new opportunities for effectively, timely, and affordable services. Patient satisfaction can be a good indicator as it reaches the highest levels. According to the statistics, 79% of patients find scheduling a follow-up visit via the eHealth applications rather convenient than an in-person visit arrangement.
At the same time, there’s less chance that they can miss such appointments due to the long distance to the clinic, time spent in waiting rooms, additional expenses, etc. Video calls are conducted at any convenient time and can take less than 30 minutes. Moreover, healthcare providers considerably decrease the workload of the busiest hospital and devote extra time to high-risk patients.
Regarding telehealth software development, it is a win-win solution all around. The real value is the connection between all the users involved in the healthcare chain and how they can really benefit from it. Patients and doctors that are the main participants in healthcare have become two active users of eHealth. More and more people would rather apply for the service of physicians, therapists, psychologists, and nurse practitioners via the Doctor On Demand applications. Whereas doctors acknowledge the exceptional functionality like EHR and EMR, ePrescriptions, laboratory tests, medical calculations, etc.
Let’s define what important telehealth features to include here.
TELEHEALTH SOFTWARE FEATURES
Telehealth software development would cover the needs of the two main actors types: patients and medical personnel. There is also clinic administration staff, but their functionality is not essential for the eHealth software to function, so it will be covered briefly.
Now that we have defined two main users, it is much easier to decide on the required functionalities. To start with, a telehealth software developer deals with complex systems of integrated hospital management system modules, including separate applications for doctors and patients. It would be an obvious thing that app features are chosen according to user roles in healthcare. So let’s outline the most common features for both of these eHealth applications.
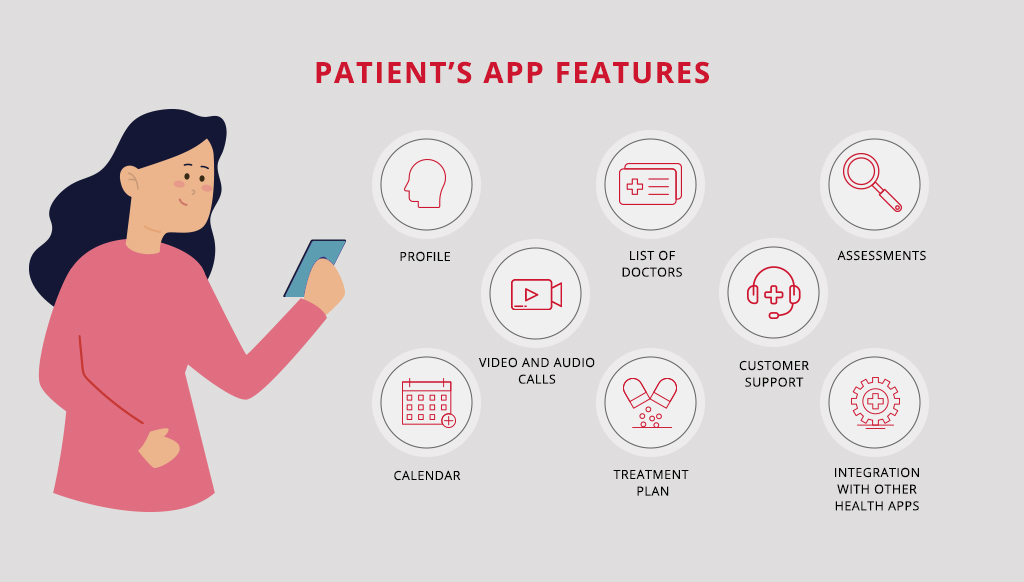
TELEHEALTH FEATURES FOR PATIENTS
It is important to develop functional and user-centered software that will cover the patient’s needs and be oriented on their convenience and accessibility. Both healthcare providers and development teams have to anticipate customer requirements and meet them with the following functionalities.
User profile
Besides containing general information like name, age, or address, patients need to have access to data on last visits, lab orders, results, prescriptions, treatment guides, etc. It is always great to add the search for insurance providers to check if the patient is covered or the employer section as many of them reimburse costs for video visits as well.
List of the doctors
The great search engine allows patients to find the required specialists just in a few clicks. Firstly, doctors need to be categorized by specialty, current availability, and location. It isn’t just convenient that the patient can schedule the follow-up appointment in a clinic, but it can be limited by state laws like in the US. Doctors licensed in certain states can’t serve the patient from others until they get their licenses as well. Specialists’ rates via patient feedback are a great addition to improving the quality and transparency of the services.
Assessments
That is one of the nice-to-have telehealth features that helps in the pre-diagnosis stage and treatment itself. The functionality is quite diverse. As far as filling in the simple questionnaire, the patient knows what specialists to contact, or doctors can gather necessary data on the current patient’s condition before the video visit or call. The more details the specialists gather, the more accurate diagnosis is made.
Video and audio calls
Real-time interaction enables medical practitioners to serve at a distance. That is an efficient solution for primary, preventative, or chronic care. It is important to understand that making a call via telehealth video conferencing software is completely different from the regular telecommunication app. Each transmission is secure and HIPAA compliant, as it has to be during the in-person visit.
Customer support
It is required to provide the technical support that raises customer engagement, solves disputes between patients and doctors, and conducts negotiations on service, payment, and insurance-related questions. Moreover, the development team has to find solutions to moderate software platforms, including user feedback, doctors’ workload, etc. For example, tracking the visits’ actuality is rather important, so the patients aren’t charged for canceled or missed visits, and doctors aren’t paid for services that they don’t provide.
Calendar
The advanced calendar would be a great addition to the functional telehealth software system. Patients would benefit from the customized designs, synchronization with other calendars, and integration with scheduling features of doctor portals. It allows users to easily find free appointment slots due to doctors’ availability, schedule calls/video visits, and sets automatic reminders on upcoming events. Moreover, this app feature can become a customized tool to develop and maintain healthy habits like physical activities, a sleep schedule, staying hydrated, and taking medicine on time. The more features you add, the better time management tool you present for your users. One thing to remember here is being complex under the hood; it has to be clear and easy to use for patients.
Treatment plan
eHealth application by default should not only provide patients with effective ways of diagnostics and treatment prescription but also a convenient way to follow doctor’s recommendations. This functionality aims at assisting patients while they undergo treatment. Besides the detailed doctors’ guidance, automatic reminders are sent every time patients have to take pills, do exercises, run lab tests, and have the next check with the doctor. It ensures better patient engagement and helps the medical staff monitor the changes and improvements in patient health conditions.
Integration with other eHealth applications
If the app synchronizes with other applications, gathered data becomes a valuable source that helps medical personnel make a more accurate diagnosis. For example, the HealthKit application reads and writes the health data like temperature, blood pressure, oxygen saturation, and blood glucose. Permitting to share it with the primary care provider allows them to monitor patients’ conditions regularly.
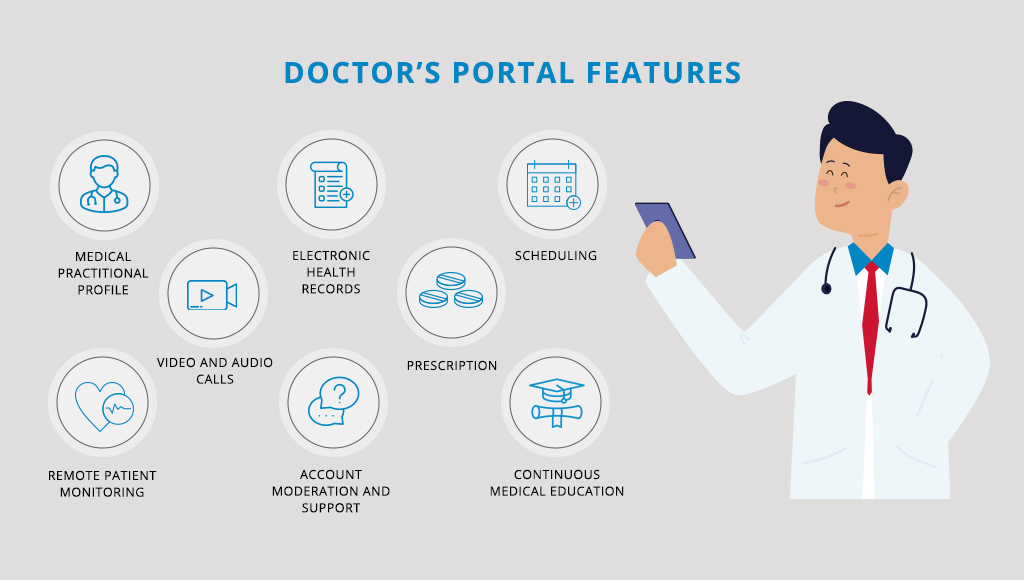
TELEHEALTH FEATURES FOR DOCTORS
In order to provide quality services for patients, medical practitioners have to be equipped with professional tools. In the case of eHealth, it is advanced software that enables connections between the involved parties. So let’s define the most common functionalities to include here.
Medical practitioner profile
The doctor’s profile is like a resume that would be presented to patients and other healthcare providers. The more complete the profile is, the more professional and trusting it looks. The appropriate professional photos, past experience, licenses and certifications, and best accomplishments have to be covered here. It is always a great idea to include customers’ feedback and rates.
Electronic health records
Like any other application for healthcare professionals, it has to be fully integrated with EHR and EMR systems. This ensures valued-based care within regulatory compliance and enables secure data exchange with patients, and third-party providers like pharmacies, insurance services, health registries, etc. For example, doctors can get access to the disease history, previously prescribed treatments, reports on patients’ lab test results, and health improvement data gathered by other eHealth applications.
Scheduling
Using in-built features, the physicians are able to manage their timetable, schedule calls, and video visits, track working hours, etc. Integration with Google Calendar, iCalendar, or other time management apps advances the overall app functionality. Automated reminders allow doctors to be on schedule everywhere and inform patients about open hours to book appointments. Moreover, telehealth software systems can gather data on the busiest hours to offer better specialists’ availability.
Video and audio calls
Remaining the main feature of any telehealth software system, it targets establishing direct communication between doctors and patients through HQ Audio or/and HQ Video. The development team also has to implement video and audio recordings and hosting features. Besides, it is essential to provide good video compression to save Internet traffic or dial-in numbers to connect via voice using a regular phone. Quite often during the call, the medical personnel needs access to doctor’s notes, medical protocols, and calculators, treatment guidance. Considering that fact, the additional functionality is a necessity to consult patients on the highest level.
Prescription
It is a common practice to suggest complete drug info, brand, pricing, and the closest pharmacies with available medicine. Once the ePrescription is written, it can be shared with both patients and pharmacy services. Nevertheless, all the prescriptions have to comply with the necessary regulations. For example, the ePrescription for controlled substances like codeine is forbidden as it is only done after visiting the doctor in person.
Remote patient monitoring
The advanced telehealth features bring together many connected tools to deliver higher-quality care services. A centralized repository gathers the patients’ data via sensors, wearables or other synchronized apps to process and share with healthcare providers. It enables improved support, daily awareness of patients’ conditions as well as emergency prevention. Ensuring better patient and doctor engagement is the main target of any healthcare system.
Account moderation and support
Medical practitioners are usually granted additional permissions to perform actions. Account moderation and support would help to build good relationships within the app community. For example, doctors also have the ability to moderate the chats. It can cover no posting from guests, only signed-in users, limited history and embedded access, and denied permissions to post messages or share images. Sometimes it even ends up blocking certain users. However, it could prevent policy violations and solve disputes arising.
Continuous medical education
An extremely helpful tool can include different case studies, practice-changing updates as well as sharing experiences with doctors that use the same software. In other words, it’s building a progressive and supportive community within your app. For example, the telehealth software development team can include an internal chat for medical specialists to share their first-hand experience or quick mass mailing updates about some new methodology or medicine.
Want some more information on the features and modules of a healthcare system?
Read the article about the features and modules of a hospital management system. In the article, you’ll also find the advantages of such software in the modern world.
HIPAA COMPLIANCE FOR TELEHEALTH SOFTWARE DEVELOPMENT
While eHealth improves the mobility and efficiency of healthcare services, it also increases the security risks associated with medical data protection. Unless telehealth software development adopts the safety regulations, it can’t be legitimate. The adoption is strictly governed by state, federal, and international laws. Anyone providing healthcare services and service-related operations like payment and support are under provisions of the Health Insurance Portability and Accountability Act (HIPAA). It was introduced in US legislation in 1996 to protect medical data, regulate transmissions, and limit access to unauthorized entities.
The regulations focus on physical, procedural, and network security measures taken by both covered entities and business associates. The important thing is that companies are free to choose the approaches suitable for their telehealth software development process as long as they remain in compliance with HIPAA. Here are some of the good practices to consider while developing HIPPA-compliant software for telehealth.
- Access control – Establishing the procedure of managing document, file, and image exchange is a great decision as files are assigned security-level labels and remain accessible only to authorized users.
- Encryption – Following FIPS 140-2 is strongly recommended for HIPAA-compliant telehealth software platforms.
- Audit controls and activity logs – These are common technical safeguards to control and record activities done with the data after its access.
- Automatic log-off and two steps user verification – The simple features that prevent unauthorized users from getting access when devices are not watched or in the cases of the user’s credentials stealing.
- Risk assessment – Both healthcare providers and development teams have to identify hazards and risk factors and determine appropriate ways to eliminate them.
- Restricted third-party access – Any medical data can’t be processed, transferred, and held by third-party services until partners sign Business Associate Agreements.
- Contingency plan – In case of emergency, the developed plan enables continuing business processes and integrity protection. Moreover, backup copies prevent sensitive data loss.
- Security incident report – Constant reporting gives a higher chance to counteract possible breaches.
All the security measures have to be documented while covering key aspects considered in risk assessment. It is also recommended to provide special training to inform medical personnel and other employees about the security policies to decrease the risks of sharing data outside the organization.
Failure or refusal to develop HIPPA-compliant software for telehealth has serious consequences. Healthcare organizations, as well as their employees, can be fined by violating rules. Among the first reached settlements with the covered entity was the CVS pharmacy fined $2.25 million for improper data exposure. Besides civil penalties, some violations like data use for personal gain, and selling data are considered due to criminal charges and prison terms.
How to start healthcare app development?
We also suggest checking the comprehensive guide with other decisive aspects to deliver successful healthcare applications.
TELEHEALTH SOFTWARE DEVELOPMENT TRENDS
Telehealth software development has grown significantly recently, especially due to continuous technological advancement. Some of the top telehealth software development trends include:
Mobile applications: Mobile apps are becoming increasingly popular for telehealth services. Patients can use telehealth apps to schedule virtual appointments, communicate with healthcare providers, and manage their health information. Telehealth apps can also integrate with wearable devices and other health monitoring tools to provide patients with a comprehensive view of their health.
Cloud-based platforms: Cloud-based telehealth platforms offer scalability and flexibility, allowing healthcare providers to access patient data and communicate with patients from anywhere with an internet connection. Cloud-based platforms can also offer enhanced security features and compliance with regulations such as HIPAA. Additionally, they can provide data analytics capabilities to help healthcare providers identify trends and optimize their services.
Wearable devices: Wearable devices such as smartwatches, fitness trackers, and biosensors are becoming increasingly popular for telehealth applications. Patients can use them to monitor their health status in real time and transmit data to healthcare providers for analysis. For example, patients with chronic conditions such as diabetes or hypertension can use wearable devices to monitor their blood glucose or blood pressure levels, while athletes can use them to monitor their fitness and performance.
Artificial Intelligence and Machine Learning: ML and AI algorithms can analyze patient data such as medical history, symptoms, and test results to provide more accurate diagnoses and personalized treatment plans. They can also assist with identifying and managing chronic diseases, detecting potential health risks, and predicting outcomes. For example, AI-powered chatbots can help patients with common health concerns, while ML algorithms can help identify patients at risk of developing certain conditions such as diabetes or heart disease.
Virtual Reality and Augmented Reality: AR and VR technologies can be used for patient education, pain management, and even surgical training. VR and AR simulations can provide patients with an interactive and immersive experience, allowing them to better understand their condition and treatment options. For example, VR can be used for physical therapy exercises or to provide distraction during medical procedures, while AR can be used to assist surgeons during operations.
Integration with EHR and EMR systems: Integrating telehealth platforms with these systems can streamline the exchange of patient information between healthcare providers. This can improve care coordination and reduce errors and duplicative testing. Additionally, integrating can help ensure that patient data is safe and compliant with HIPAA regulations.
Overall, these telehealth software development trends aim to improve patient outcomes, increase access to healthcare services, and leverage technology to enhance the healthcare experience for patients and healthcare providers. By adopting these trends, healthcare providers can offer patients more personalized, efficient, and effective care.
CONCLUSION
Healthcare, primarily limited to hospitals, is changing its extensions at a rapid pace. Telehealth software development has become vital for inpatient and outpatient care. Efficient, accessible, and affordable health services are much needed for modern society. If you want to know the approximate development cost and timeline, read the article about telemedicine software cost. It also covers the topic of technology choice.
Specialists of Existek have all the necessary tools and technologies to implement a solution for the healthcare industry. Covering the needs of all involved parties, gathering the professional development team, and using up-to-date technologies enable your products and services to succeed. We hope this article has helped define the important functionality for telehealth software development and given practical advice on your security solutions.
Have additional questions about how to create telehealth solutions?
Please do not hesitate to contact Existek. We are an outsourcing software development company with extensive experience in the healthcare industry. We focus on providing the best quality services and finding reasonable solutions for our customers.
Frequently asked questions
What is telehealth software development?
Telehealth software development involves creating software applications or platforms that allow healthcare providers and patients to communicate and access medical services remotely. Telehealth software development enables medical professionals to provide remote medical care, consultation, and monitoring using various digital tools such as video conferencing, chat, remote monitoring, etc.
What major types of healthcare services does telehealth cover?
The main types of services focus on the following:
Store-and-forward
Remote monitoring
Real-time interaction
What features do telehealth solutions have?
Telehealth features for patients: user profile, list of the doctors, assessments, video and audio calls, customer support, calendar, treatment plan, and integration with other eHealth apps.
Telehealth features for doctors: medical practitioner profile, electronic health records, scheduling, video and audio calls, prescriptions, remote patient monitoring, account moderation and support, and continuous medical education.
What are telehealth software development trends?
It’s worth saying that the telehealth market has greatly evolved over the recent years with great potential for the future. The main trends include the following:
Mobile applications
Cloud-based platforms
Wearable devices
Increased use of AI and ML
VR and AR
Integration with EHR and EMR systems